Background:
Myeloproliferative neoplasms (MPNs) are clonal hematopoietic disorders associated with elevated thrombotic and bleeding risk. Contemporary care has led to comparable lifespans between patients with MPNs and the general population; thus, surgical procedures for degenerative arthritis including total hip arthroplasty (THA) and total knee arthroplasty (TKA) are becoming more common among patients with MPNs. Lower extremity arthroplasty carries considerable thrombotic risk in the general population but estimates for the thrombotic and bleeding complications in patients with MPNs are lacking.
Methods:
We performed a population-based, propensity-matched retrospective cohort study utilizing data from a MarketScan database to compare 30-day rates of postoperative venous thromboembolism (VTE) and bleeding in THA/TKA patients with MPNs. We included patients undergoing primary THA/TKA with continuous insurance enrollment 3 months prior to surgery. We identified patients with MPNs utilizing ICD-10 codes. Validated algorithms of claims codes were used to label comorbidities including obesity, chronic kidney disease, cancer, inherited thrombophilias, antiphospholipid antibody, or lupus anticoagulant. Primary outcomes included cumulative incidence rates of postoperative VTE and bleeding at 30 days. Logistic regression was utilized to assess for an association between MPN diagnosis and outcomes in the overall cohort, presented as an odds ratio (OR) with a 95% confidence interval (CI). Propensity score matching was utilized to match each patient with MPNs to controls (1:3) using a scoring algorithm calculated based on age, sex, comorbidities (including prior VTE, obesity, cancer, chronic kidney disease, THA/TKA, length of stay, inherited thrombophilias, antiphospholipid antibody, or lupus anticoagulant) and thromboprophylactic medication. We further utilized a logistic regression analysis to identify factors independently associated with 30-day VTE and bleeding in patients with MPN undergoing THA/TKA.
Results:
Of a total of 131,566 eligible patients, 598 (0.4%) patients with MPNs with a median age of 61 years (IQR 56-66), 65% women, and 60% TKA were included. The majority had essential thrombocythemia (72%), and polycythemia vera (21%). Comorbid conditions included obesity (30%), chronic kidney disease (9%), cancer (8%), and prior VTE (6%). There were 20 thrombotic events within 30 days after arthroplasty among patients with MPNs including 16 deep vein thrombosis and 4 pulmonary embolism events.
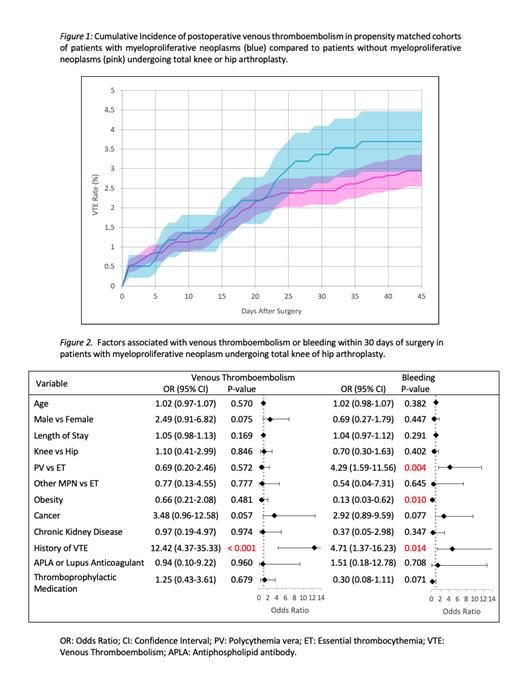
After adjusting for age, gender, type of surgery, comorbidities, length of stay, and thromboprophylaxis, a MPN diagnosis was not associated with 30-day VTE (OR 1.3, 95% CI 0.8-2.1, P=0.2) or bleeding (OR 1.2, 95% CI 0.8-1.8, P=0.4). The postsurgical cumulative incidence rates of VTE in patients with MPNs (3.37%, 95% CI 2.63-4.11) did not significantly differ in the propensity-matched comparison group of 1,763 patients without MPNs (2.4%, 95% CI 2.1-2.8), (OR 1.4, 95% CI 0.8-2.5 P=0.2) (Figure 1). There was no significant difference in the postsurgical rates of bleeding in patients with MPNs (3.9%, 95% CI 3.1-4.7) compared to patients without MPNs (3.1%, 95% CI 2.7-3.5), (OR 1.3, 0.8-2.2 P=0.2). History of VTE was the only independent risk factor associated with postoperative VTE at 30 days (OR 12.42, 95% CI 4.4-35.3) (Figure 2). Factors associated with bleeding included polycythemia vera (OR 4.29, 95% CI 1.6-11.6), obesity (OR 0.13, 95% CI 0.03-0.6, P=0.01), and prior history of VTE (OR 4.7, 95% CI 1.4-16.2) (Figure 2).
Conclusion:
In this large claims-based database, patients with MPNs undergoing TKA and THA did not have significantly higher rates of postoperative VTE or bleeding. Among patients with MPNs undergoing lower extremity arthroplasty, prior history of VTE was the only factor significantly associated with postsurgical thrombosis. Specific MPN subtypes were not associated with a differential thrombotic risk but did impact post-operative bleeding. Characterization of these outcomes could lead to a better assessment of the surgical risk factors affecting this population and eventually aid clinicians in optimizing thromboprophylaxis for this high-risk group.
Disclosures
Zwicker:calyx: Consultancy; Sanofi, CSL, Parexel: Consultancy; Pfizer/BMS, Portola, Daiichi: Honoraria; Sanofi: Consultancy; Janssen: Consultancy; Incyte Corporation, Quercegen: Research Funding; CSL Behring: Consultancy. Flaumenhaft:Cleveland KUH- Training network: Honoraria, Membership on an entity's Board of Directors or advisory committees; Function Therapeutics: Membership on an entity's Board of Directors or advisory committees; Porosome Therapeutics: Current equity holder in private company, Membership on an entity's Board of Directors or advisory committees; Versiti Blood Research Center: Membership on an entity's Board of Directors or advisory committees; Xap Therapeutics: Consultancy; Platelet Diagnostics: Consultancy, Current equity holder in private company, Patents & Royalties.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal